download (or) read freely educational topics
Read or simply take a screen shot for reading after closing the web (or) turning of mobile data
Friday, July 24, 2020
digestive system for neet attenders
Digestive Processes
The processes of digestion include six activities: ingestion, propulsion, mechanical or physical digestion, chemical digestion, absorption, and defecation.
The first of these processes, ingestion, refers to the entry of food into the alimentary canal through the mouth. There, the food is chewed and mixed with saliva, which contains enzymes that begin breaking down the carbohydrates in the food plus some lipid digestion via lingual lipase. Chewing increases the surface area of the food and allows an appropriately sized bolus to be produced.

Figure 1. Peristalsis moves food through the digestive tract with alternating waves of muscle contraction and relaxation.
Food leaves the mouth when the tongue and pharyngeal muscles propel it into the esophagus. This act of swallowing, the last voluntary act until defecation, is an example of propulsion, which refers to the movement of food through the digestive tract. It includes both the voluntary process of swallowing and the involuntary process of peristalsis. Peristalsis consists of sequential, alternating waves of contraction and relaxation of alimentary wall smooth muscles, which act to propel food along (Figure 1). These waves also play a role in mixing food with digestive juices. Peristalsis is so powerful that foods and liquids you swallow enter your stomach even if you are standing on your head.
Digestion includes both mechanical and chemical processes. Mechanical digestion is a purely physical process that does not change the chemical nature of the food. Instead, it makes the food smaller to increase both surface area and mobility. It includes mastication, or chewing, as well as tongue movements that help break food into smaller bits and mix food with saliva. Although there may be a tendency to think that mechanical digestion is limited to the first steps of the digestive process, it occurs after the food leaves the mouth, as well. The mechanical churning of food in the stomach serves to further break it apart and expose more of its surface area to digestive juices, creating an acidic “soup” called chyme. Segmentation, which occurs mainly in the small intestine, consists of localized contractions of circular muscle of the muscularis layer of the alimentary canal. These contractions isolate small sections of the intestine, moving their contents back and forth while continuously subdividing, breaking up, and mixing the contents. By moving food back and forth in the intestinal lumen, segmentation mixes food with digestive juices and facilitates absorption.
In chemical digestion, starting in the mouth, digestive secretions break down complex food molecules into their chemical building blocks (for example, proteins into separate amino acids). These secretions vary in composition, but typically contain water, various enzymes, acids, and salts. The process is completed in the small intestine.
Food that has been broken down is of no value to the body unless it enters the bloodstream and its nutrients are put to work. This occurs through the process of absorption, which takes place primarily within the small intestine. There, most nutrients are absorbed from the lumen of the alimentary canal into the bloodstream through the epithelial cells that make up the mucosa. Lipids are absorbed into lacteals and are transported via the lymphatic vessels to the bloodstream (the subclavian veins near the heart). The details of these processes will be discussed later.
In defecation, the final step in digestion, undigested materials are removed from the body as feces.
AGING AND THE DIGESTIVE SYSTEM: FROM APPETITE SUPPRESSION TO CONSTIPATION
Age-related changes in the digestive system begin in the mouth and can affect virtually every aspect of the digestive system. Taste buds become less sensitive, so food isn’t as appetizing as it once was. A slice of pizza is a challenge, not a treat, when you have lost teeth, your gums are diseased, and your salivary glands aren’t producing enough saliva. Swallowing can be difficult, and ingested food moves slowly through the alimentary canal because of reduced strength and tone of muscular tissue. Neurosensory feedback is also dampened, slowing the transmission of messages that stimulate the release of enzymes and hormones.
Pathologies that affect the digestive organs—such as hiatal hernia, gastritis, and peptic ulcer disease—can occur at greater frequencies as you age. Problems in the small intestine may include duodenal ulcers, maldigestion, and malabsorption. Problems in the large intestine include hemorrhoids, diverticular disease, and constipation. Conditions that affect the function of accessory organs—and their abilities to deliver pancreatic enzymes and bile to the small intestine—include jaundice, acute pancreatitis, cirrhosis, and gallstones.
In some cases, a single organ is in charge of a digestive process. For example, ingestion occurs only in the mouth and defecation only in the anus. However, most digestive processes involve the interaction of several organs and occur gradually as food moves through the alimentary canal (Figure 2).
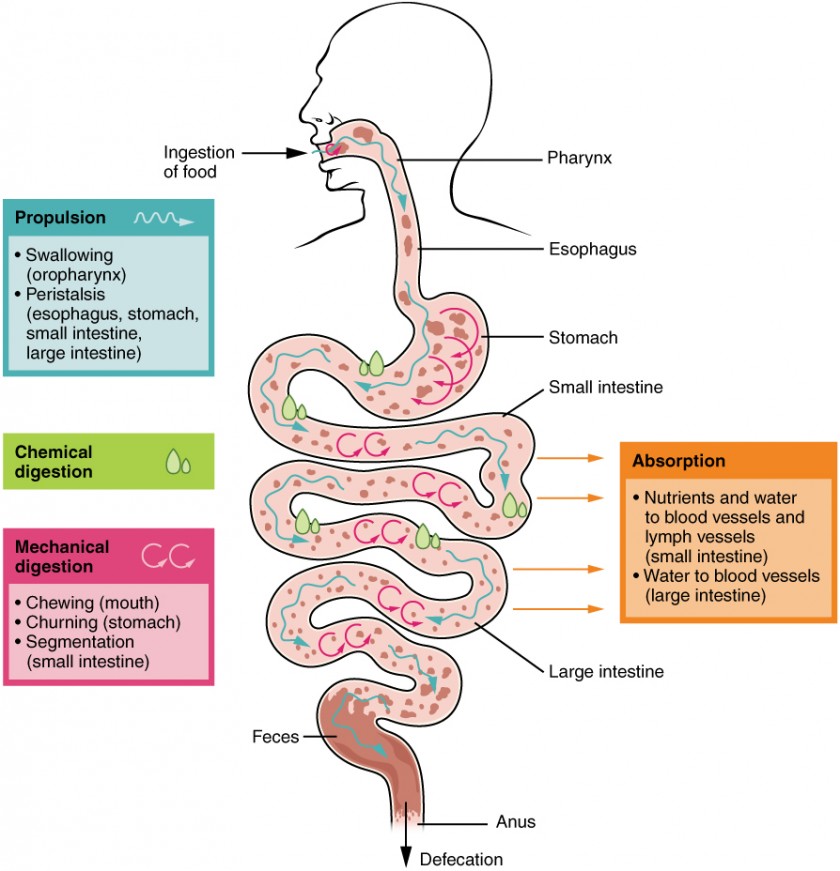
Figure 2. The digestive processes are ingestion, propulsion, mechanical digestion, chemical digestion, absorption, and defecation.
Some chemical digestion occurs in the mouth. Some absorption can occur in the mouth and stomach, for example, alcohol and aspirin.
Regulatory Mechanisms
Neural and endocrine regulatory mechanisms work to maintain the optimal conditions in the lumen needed for digestion and absorption. These regulatory mechanisms, which stimulate digestive activity through mechanical and chemical activity, are controlled both extrinsically and intrinsically.
Neural Controls
The walls of the alimentary canal contain a variety of sensors that help regulate digestive functions. These include mechanoreceptors, chemoreceptors, and osmoreceptors, which are capable of detecting mechanical, chemical, and osmotic stimuli, respectively. For example, these receptors can sense when the presence of food has caused the stomach to expand, whether food particles have been sufficiently broken down, how much liquid is present, and the type of nutrients in the food (lipids, carbohydrates, and/or proteins). Stimulation of these receptors provokes an appropriate reflex that furthers the process of digestion. This may entail sending a message that activates the glands that secrete digestive juices into the lumen, or it may mean the stimulation of muscles within the alimentary canal, thereby activating peristalsis and segmentation that move food along the intestinal tract.
The walls of the entire alimentary canal are embedded with nerve plexuses that interact with the central nervous system and other nerve plexuses—either within the same digestive organ or in different ones. These interactions prompt several types of reflexes. Extrinsic nerve plexuses orchestrate long reflexes, which involve the central and autonomic nervous systems and work in response to stimuli from outside the digestive system. Short reflexes, on the other hand, are orchestrated by intrinsic nerve plexuses within the alimentary canal wall. These two plexuses and their connections were introduced earlier as the enteric nervous system. Short reflexes regulate activities in one area of the digestive tract and may coordinate local peristaltic movements and stimulate digestive secretions. For example, the sight, smell, and taste of food initiate long reflexes that begin with a sensory neuron delivering a signal to the medulla oblongata. The response to the signal is to stimulate cells in the stomach to begin secreting digestive juices in preparation for incoming food. In contrast, food that distends the stomach initiates short reflexes that cause cells in the stomach wall to increase their secretion of digestive juices.
Hormonal Controls
A variety of hormones are involved in the digestive process. The main digestive hormone of the stomach is gastrin, which is secreted in response to the presence of food. Gastrin stimulates the secretion of gastric acid by the parietal cells of the stomach mucosa. Other GI hormones are produced and act upon the gut and its accessory organs. Hormones produced by the duodenum include secretin, which stimulates a watery secretion of bicarbonate by the pancreas; cholecystokinin (CCK), which stimulates the secretion of pancreatic enzymes and bile from the liver and release of bile from the gallbladder; and gastric inhibitory peptide, which inhibits gastric secretion and slows gastric emptying and motility. These GI hormones are secreted by specialized epithelial cells, called endocrinocytes, located in the mucosal epithelium of the stomach and small intestine. These hormones then enter the bloodstream, through which they can reach their target organs.
Chapter Review
The digestive system ingests and digests food, absorbs released nutrients, and excretes food components that are indigestible. The six activities involved in this process are ingestion, motility, mechanical digestion, chemical digestion, absorption, and defecation. These processes are regulated by neural and hormonal mechanisms.
Anatomy and Circulation of the Heart
Your heart is an amazing organ. It continuously pumps oxygen and nutrient-rich blood throughout your body to sustain life. This fist-sized powerhouse beats (expands and contracts) 100,000 times per day, pumping five or six quarts of blood each minute, or about 2,000 gallons per day.
How Does Blood Travel Through the Heart?
As the heart beats, it pumps blood through a system of blood vessels, called the circulatory system. The vessels are elastic tubes that carry blood to every part of the body.
Blood is essential. In addition to carrying fresh oxygen from the lungs and nutrients to your body's tissues, it also takes the body's waste products, including carbon dioxide, away from the tissues. This is necessary to sustain life and promote the health of all the body's tissues.
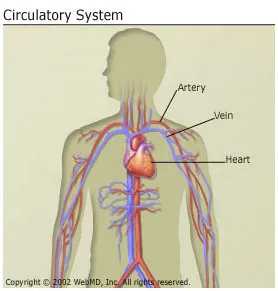
There are three main types of blood vessels:
- Arteries. They begin with the aorta, the large artery leaving the heart. Arteries carry oxygen-rich blood away from the heart to all of the body's tissues. They branch several times, becoming smaller and smaller as they carry blood farther from the heart.
- Capillaries. These are small, thin blood vessels that connect the arteries and the veins. Their thin walls allow oxygen, nutrients, carbon dioxide, and other waste products to pass to and from our organ's cells.
- Veins. These are blood vessels that take blood back to the heart; this blood lacks oxygen (oxygen-poor) and is rich in waste products that are to be excreted or removed from the body. Veins become larger and larger as they get closer to the heart. The superior vena cava is the large vein that brings blood from the head and arms to the heart, and the inferior vena cava brings blood from the abdomen and legs into the heart.
This vast system of blood vessels -- arteries, veins, and capillaries -- is over 60,000 miles long. That's long enough to go around the world more than twice!
Blood flows continuously through your body's blood vessels. Your heart is the pump that makes it all possible.
Where Is Your Heart and What Does It Look Like?
The heart is located under the rib cage, to the left of your breastbone (sternum) and between your lungs.
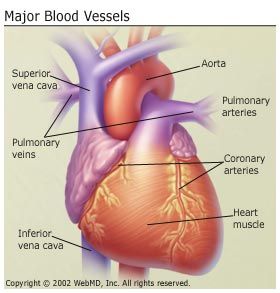
Looking at the outside of the heart, you can see that the heart is made of muscle. The strong muscular walls contract (squeeze), pumping blood to the arteries. The major blood vessels connected to your heart are the aorta, the superior vena cava, the inferior vena cava, the pulmonary artery (which takes oxygen-poor blood from the heart to the lungs where it is oxygenated), the pulmonary veins (which bring oxygen-rich blood from the lungs to the heart), and the coronary arteries (which supply blood to the heart muscle).
On the inside, the heart is a four-chambered, hollow organ. It is divided into the left and right side by a wall called the septum. The right and left sides of the heart are further divided into two top chambers called the atria, which receive blood from the veins, and two bottom chambers called ventricles, which pump blood into the arteries.
The atria and ventricles work together, contracting and relaxing to pump blood out of the heart. As blood leaves each chamber of the heart, it passes through a valve. There are four heart valves within the heart:
- Mitral valve
- Tricuspid valve
- Aortic valve
- Pulmonic valve (also called pulmonary valve)
The tricuspid and mitral valves lie between the atria and ventricles. The aortic and pulmonic valves lie between the ventricles and the major blood vessels leaving the heart.
The heart valves work the same way as one-way valves in the plumbing of your home. They prevent blood from flowing in the wrong direction.
Each valve has a set of flaps, called leaflets or cusps. The mitral valve has two leaflets; the others have three. The leaflets are attached to and supported by a ring of tough, fibrous tissue called the annulus. The annulus helps to maintain the proper shape of the valve.
The leaflets of the mitral and tricuspid valves are also supported by tough, fibrous strings called chordae tendineae. These are similar to the strings supporting a parachute. They extend from the valve leaflets to small muscles, called papillary muscles, which are part of the inside walls of the ventricles.
How Does Blood Flow Through the Heart?
The right and left sides of the heart work together. The pattern described below is repeated over and over, causing blood to flow continuously to the heart, lungs, and body.
Right side
- Blood enters the heart through two large veins, the inferior and superior vena cava, emptying oxygen-poor blood from the body into the right atrium.
- As the atrium contracts, blood flows from your right atrium into your right ventricle through the open tricuspid valve.
- When the ventricle is full, the tricuspid valve shuts. This prevents blood from flowing backward into the atria while the ventricle contracts.
- As the ventricle contracts, blood leaves the heart through the pulmonic valve, into the pulmonary artery and to the lungs where it is oxygenated.
Left side
- The pulmonary vein empties oxygen-rich blood from the lungs into the left atrium.
- As the atrium contracts, blood flows from your left atrium into your left ventricle through the open mitral valve.
- When the ventricle is full, the mitral valve shuts. This prevents blood from flowing backward into the atrium while the ventricle contracts.
- As the ventricle contracts, blood leaves the heart through the aortic valve, into the aorta and to the body.
How Does Blood Flow Through Your Lungs?
Once blood travels through the pulmonic valve, it enters your lungs. This is called the pulmonary circulation. From your pulmonic valve, blood travels to the pulmonary artery to tiny capillary vessels in the lungs.
Here, oxygen travels from the tiny air sacs in the lungs, through the walls of the capillaries, into the blood. At the same time, carbon dioxide, a waste product of metabolism, passes from the blood into the air sacs. Carbon dioxide leaves the body when you exhale. Once the blood is purified and oxygenated, it travels back to the left atrium through the pulmonary veins.
What Are the Coronary Arteries?
Like all organs, your heart is made of tissue that requires a supply of oxygen and nutrients. Although its chambers are full of blood, the heart receives no nourishment from this blood. The heart receives its own supply of blood from a network of arteries, called the coronary arteries.
Two major coronary arteries branch off from the aorta near the point where the aorta and the left ventricle meet:
- Right coronary artery supplies the right atrium and right ventricle with blood. It usually branches into the posterior descending artery, which supplies the bottom portion of the left ventricle and back of the septum with blood.
- Left main coronary artery branches into the circumflex artery and the left anterior descending artery. The circumflex artery supplies blood to the left atrium, side, and back of the left ventricle, and the left anterior descending artery supplies the front and bottom of the left ventricle and the front of the septum with blood.
These arteries and their branches supply all parts of the heart muscle with blood.
When the coronary arteries narrow to the point that blood flow to the heart muscle is limited (coronary artery disease), a network of tiny blood vessels in the heart that aren't usually open called collateral vessels may enlarge and become active. This allows blood to flow around the blocked artery to the heart muscle, protecting the heart tissue from injury.
How Does the Heart Beat?
The atria and ventricles work together, alternately contracting and relaxing to make the heart beat and pump blood. The electrical system of your heart is the power source that makes this possible.
Your heartbeat is triggered by electrical impulses that travel down a special pathway through your heart.
- The impulse starts in a small bundle of specialized cells called the SA node (sinoatrial node), located in the right atrium. This node is known as the heart's natural pacemaker. The electrical activity spreads through the walls of the atria and causes them to contract.
- A cluster of cells in the center of the heart between the atria and ventricles, the AV node (atrioventricular node) is like a gate that slows the electrical signal before it enters the ventricles. This delay gives the atria time to contract before the ventricles do.
- The His-Purkinje network is a pathway of fibers that sends the impulse to the muscular walls of the ventricles, causing them to contract.
At rest, a normal heart beats around 50 to 99 times a minute. Exercise, emotions, fever, and some medications can cause your heart to beat faster, sometimes to well over 100 beats per minute.
